The impact of the COVID-19 pandemic on cardiovascular disease prevention and management
Published: 23 January 2023
Nearly half a million people missed out on starting medication to lower their blood pressure during COVID19 pandemic - important new research led by BHFDataScience published in NatureMedicine co-authored by SCMH's Prof Naveed Sattar.
Caroline E. Dale, Rohan Takhar, Raymond Carragher, Michail Katsoulis, Fatemeh Torabi, Stephen Duffield, Seamus Kent, Tanja Mueller, Amanj Kurdi, Thu Nguyen Le Anh, Stuart McTaggart, Hoda Abbasizanjani, Sam Hollings, Andrew Scourfield, Ronan A. Lyons, Rowena Griffiths, Jane Lyons, Gareth Davies, Daniel Harris, Alex Handy, Mehrdad A. Mizani, Christopher Tomlinson, Johan H. Thygesen, Mark Ashworth, Spiros Denaxas, Amitava Banerjee, Jonathan A. C. Sterne, Paul Brown, Ian Bullard, Rouven Priedon, Mamas A. Mamas, Ann Slee, Paula Lorgelly, Munir Pirmohamed, Kamlesh Khunti, Andrew D. Morris, Cathie Sudlow, Ashley Akbari, Marion Bennie, Naveed Sattar, Reecha Sofat
Abstract
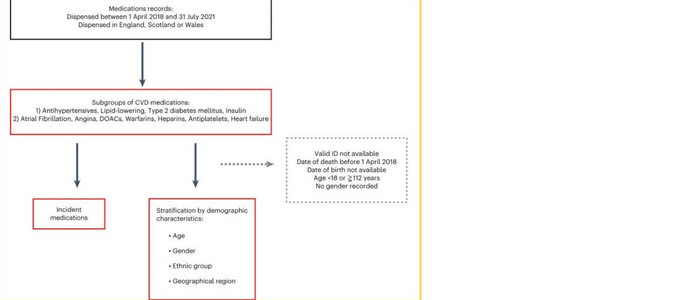
How the Coronavirus Disease 2019 (COVID-19) pandemic has affected prevention and management of cardiovascular disease (CVD) is not fully understood. In this study, we used medication data as a proxy for CVD management using routinely collected, de-identified, individual-level data comprising 1.32 billion records of community-dispensed CVD medications from England, Scotland and Wales between April 2018 and July 2021. Here we describe monthly counts of prevalent and incident medications dispensed, as well as percentage changes compared to the previous year, for several CVD-related indications, focusing on hypertension, hypercholesterolemia and diabetes.
Main
Cardiovascular disease (CVD) remains the commonest cause of mortality and morbidity worldwide; it is, therefore, vital to understand the impact of the Coronavirus Disease 2019 (COVID-19) pandemic on CVD and its risk factors. In the UK, strategies for CVD prevention include screening for health conditions and risk factors that can be modified through medication, including type 2 diabetes mellitus (T2DM), hypertension, hypercholesterolemia and atrial fibrillation (AF). When adequately controlled, such measures reduce the level of CVD in the population.
Results
Data
We studied de-identified, individual-level, population-scale data from England, Scotland and Wales accessed through the respective national Trusted Research Environments (TREs)—that is, NHS Digital’s TRE for England (referred to throughout as ‘the English TRE’), the Scottish National Safe Haven and the Secure Anonymised Information Linkage (SAIL) Databank.
Fig. 1: Flowchart showing selection of analytical datasets.
First published: 23 January 2023

