Development of a treatment selection algorithm for SGLT2
Published: 28 November 2022
Development of a treatment selection algorithm for SGLT2 and DPP-4 inhibitor therapies in people with type 2 diabetes: a retrospective cohort study
Development of a treatment selection algorithm for SGLT2 and DPP-4 inhibitor therapies in people with type 2 diabetes: a retrospective cohort study
John M Dennis PhD, Katherine G Young PhD, Andrew P McGovern, MD Bilal A Mateen, MBBS Prof Sebastian J Vollmer PhD Michael D Simpson, PhD, Prof William E Henley, PhD, Prof Rury R Holman, FMedSci Prof Naveed Sattar, MD Prof Ewan R Pearson, PhD Prof Andrew T Hattersley, DM Prof Angus G Jones, PhD, Beverley M Shields, PhD
Summary
Background
Current treatment guidelines do not provide recommendations to support the selection of treatment for most people with type 2 diabetes. We aimed to develop and validate an algorithm to allow selection of optimal treatment based on glycaemic response, weight change, and tolerability outcomes when choosing between SGLT2 inhibitor or DPP-4 inhibitor therapies.
Methods
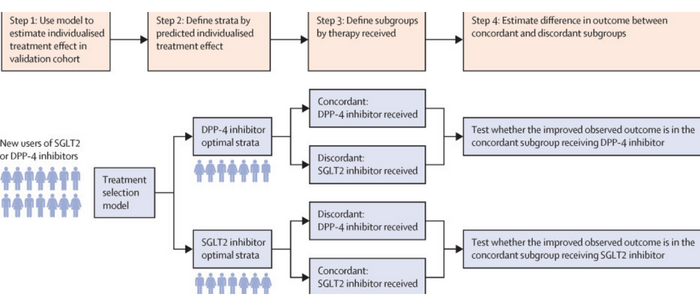
In this retrospective cohort study, we identified patients initiating SGLT2 and DPP-4 inhibitor therapies after Jan 1, 2013, from the UK Clinical Practice Research Datalink (CPRD). We excluded those who received SGLT2 or DPP-4 inhibitors as first-line treatment or insulin at the same time, had estimated glomerular filtration rate (eGFR) of less than 45 mL/min per 1·73 m2, or did not have a valid baseline glycated haemoglobin (HbA1c) measure (<53 or ≥120 mmol/mol). The primary efficacy outcome was the HbA1c value reached 6 months after drug initiation, adjusted for baseline HbA1c. Clinical features associated with differential HbA1c outcome on the two therapies were identified in CPRD (n=26 877), and replicated in reanalysis of 14 clinical trials (n=10 414). An algorithm to predict individual-level differential HbA1c outcome on the two therapies was developed in CPRD (derivation; n=14 069) and validated in head-to-head trials (n=2499) and CPRD (independent validation; n=9376). In CPRD, we further explored heterogeneity in 6-month weight change and treatment discontinuation.
Findings
Among 10 253 patients initiating SGLT2 inhibitors and 16 624 patients initiating DPP-4 inhibitors in CPRD, baseline HbA1c, age, BMI, eGFR, and alanine aminotransferase were associated with differential HbA1c outcome with SGLT2 inhibitor and DPP-4 inhibitor therapies. The median age of participants was 62·0 years (IQR 55·0–70·0). 10 016 (37·3%) were women and 16 861 (62·7%) were men. An algorithm based on these five features identified a subgroup, representing around four in ten CPRD patients, with a 5 mmol/mol or greater observed benefit with SGLT2 inhibitors in all validation cohorts (CPRD 8·8 mmol/mol [95% CI 7·8–9·8]; CANTATA-D and CANTATA-D2 trials 5·8 mmol/mol [3·9–7·7]; BI1245.20 trial 6·6 mmol/mol [2·2–11·0]). In CPRD, predicted differential HbA1c response with SGLT2 inhibitor and DPP-4 inhibitor therapies was not associated with weight change. Overall treatment discontinuation within 6 months was similar in patients predicted to have an HbA1c benefit with SGLT2 inhibitors over DPP-4 inhibitors (median 15·2% [13·2–20·3] vs 14·4% [12·9–16·7]). A smaller subgroup predicted to have greater HbA1c reduction with DPP-4 inhibitors were twice as likely to discontinue SGLT2 inhibitors than DPP-4 inhibitors (median 26·8% [23·4–31·0] vs 14·8% [12·9–16·8]).
Interpretation
A validated treatment selection algorithm for SGLT2 inhibitor and DPP-4 inhibitor therapies can support decisions on optimal treatment for people with type 2 diabetes.
Outcomes
The primary efficacy outcome was the HbA1c value reached 6 months after drug initiation, adjusted for baseline HbA1c.16 In CPRD, this outcome was defined as the closest HbA1c to 6 months after initiation (range 3–15 months) on unchanged therapy (no addition or cessation of other glucose-lowering medication and continued prescription of the drug of interest). In trials, all on treatment HbA1c values at study visits from 3–6 months after randomisation were evaluated.
Secondary outcomes in CPRD were the weight reached 6 months after initiation (closest value within 3–15 months), adjusted for baseline weight, and treatment discontinuation within 6 months of drug initiation (a proxy of drug tolerability). Patients were required to have 3 months of follow-up time after their last prescription to confirm that the drug was discontinued.
First published: 28 November 2022

