Targeted antibiotic use may help cure Chronic Myeloid Leukaemia
Published: 14 September 2017
The antibiotic tigecycline, when used in combination with current treatment, may hold the key to eradicating chronic myeloid leukaemia (CML) cells, according to new research.
The antibiotic tigecycline, when used in combination with current treatment, may hold the key to eradicating chronic myeloid leukaemia (CML) cells, according to new research.
The University of Glasgow led study, published today in Nature Medicine, demonstrates the effectiveness of combining tigecycline with the drug imatinib – a tyrosine kinase inhibitor (TKI) and standard first-line treatment of patients with CML.
Using cells isolated from CML patients, researchers showed that treatment with tigecycline, an antibiotic used to treat bacterial infection, is effective in killing CML stem cells when used in combination with imatinib. The study also shows that the novel drug combination significantly delays relapse in pre-clinical animal models of human CML.
The University of Glasgow led teams now believe that these two drugs together offer an exciting new approach to eradicate leukaemic stem cells in CML patients and potentially enhance cure rates.
Dr Vignir Helgason, joint lead author of the study who is based at the University of Glasgow, Wolfson Wohl Cancer Research Centre, said: “We were very excited to find that when we treated CML cells with both the antibiotic tigecycline and the TKI drug imatinib, CML stem cells were selectively killed.
“We believe that our findings provide a strong basis for testing this novel therapeutic strategy in clinical trials in order to eliminate CML stem cells and provide cure for CML patients.”
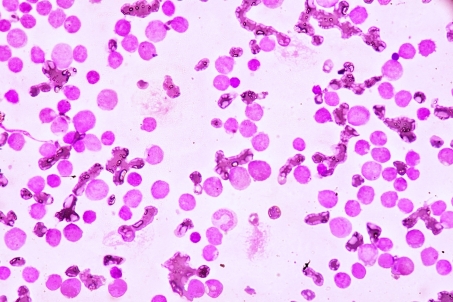
Chronic myeloid leukaemia (CML) is a form of blood cancer that turns normal blood stem cells into leukaemic stem cells, or CML stem cells. These CML stem cells then produce large numbers of leukaemic cells which, if left untreated, is fatal.
At present, CML patients are treated with tyrosine kinase inhibitors, otherwise known as TKIs, including the drug imatinib. TKIs are effective at killing the majority of the leukaemic cells, but they do not kill the CML stem cells from which the disease arises.
As a result, TKIs alone rarely cure the disease but hold its advancement at bay. Therefore, most patients need to remain on TKIs for the rest of their lives to control the disease, although with the risk of development of drug resistance. Additionally, the drugs are expensive and can cause serious side effects in some patients.
Professor Eyal Gottlieb, head for the Cancer Metabolism Research Unit at the Cancer Research UK Beatson Institute said: “Our work in this study demonstrates for the first time that CML stem cells are metabolically distinct from normal blood stem cells, and this in turn provides opportunities to selectively target them.”
Professor Karen Vousden, Cancer Research UK’s chief scientist, said: “It’s exciting to see that using an antibiotic alongside an existing treatment could be a way to keep this type of leukaemia at bay, and potentially even cure it.
“If this approach is shown to be safe and effective in humans too, it could offer a new option for patients who at the moment face long-term treatment with the possibility of relapse.
“This pioneering research was driven, in part, by Professor Holyoake, whose world leading work in CML will continue to shape research and save lives for years to come.”
World-leading CML scientist, Professor Tessa Holyoake, who was the director of the University of Glasgow Paul O’Gorman Leukaemia Research Centre who passed away recently, was also a co-author of this paper.
The study, ‘Targeting mitochondrial oxidative phosphorylation eradicates therapy-resistant chronic myeloid leukemia stem cells’, is published in Nature Medicine. The research was funded by Cancer Research UK, The Medical Research Council, AstraZeneca, Scottish Government Chief Scientist Office, The Howat Foundation, Friends of the Paul O’Gorman Leukaemia Research Centre, Bloodwise, The Kay Kendall Leukaemia Fund, Lady Tata International Award and Leuka.
First published: 14 September 2017
<< 2017

